Here is a suggestion for testing your change to ICD10 with a payer/clearinghouse
It does not matter whether you have actually used an ICD10 diagnosis code in a patient's transaction. You do not have to change your data entry to begin testing.
Note: Payer ABC wants to begin testing with ICD10. You are now successfully transmitting claims to this payer using ICD9 codes. You have just finished transmitting a claim(s) to the payer with ICD9 codes. On the main menu under #9 you have a file named: m6r964.lst (just an example). Under #10 on the main menu you have the various audits from the transmission: m6r964.trn, m6r964_837.chk, m6r964.chk (examples)
First delete all the audits under #10.
You are going to retransmit the same claims that you have in the file under #9: m6r964.lst - but this time you are going to change the ICD9 codes to ICD10. Here is how you do it:
First go the the insurance claim control screen. From the main directory select #8, #7, #3, Enter the form code (ex: 564, 964, 5gateway, 9gateway)
On the "Edit insurance control files" screen for the specific form code that you want to transmit ICD-10 codes, select the 2nd tab labeled m6r9xx.dat (where xx is assigned by you: ex: m6r964.dat or m6r9gateway.dat). In the lower right see the text box labeled 'Default diagnosis code version'. Enter ICD10 in this text box (do not enter a dash). Or you can right click and select 2 = ICD10 from the small menu.
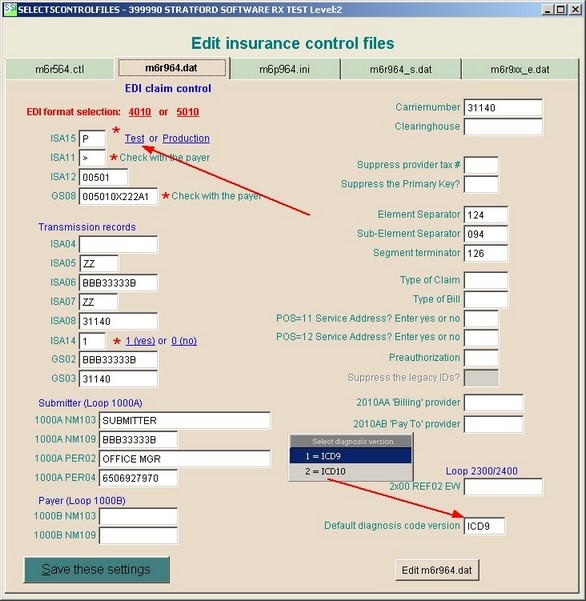
The payer may want you to transmit your test ICD10 claims in 'test' mode. If so, then you need to click the * Test link above.
Always press the 'Save these settings' button in the lower left or your changes will not be saved.
Return to the main directory and retransmit your m6r964.lst file under #9 as usual. That is all there is to it. Your same claims will be transmitted to that same payer as always, but with ICD10 diagnosis codes. Is that simple enough?
Note: after you transmit the test, you must return to the insurance control screen and un-do your changes so that your next claims will go as usual until the payer has authorized you to begin transmitting with ICD10 diagnosis codes. When you are approved, return to this manual section and make the changes above (but leave it in 'production' mode).
We would like feedback from you. Please suggest any changes that you think we should make to this section. You can even mention a specific payer and what they wanted, especially if it is something not covered in this section of the manual.