The Stratford program will send claims to thousands of payers. Even though the HIPAA law specifies how the claims should be formatted - either paper or EDI, some payers continue to have special requirements in addition (or in place of) the HIPAA requirements. It is not possible to design a data entry screen that has a place for an unlimited number of these exceptions.
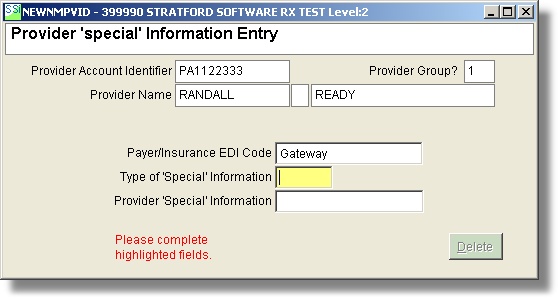
If you have a payer that wants a specific code/ID for a specific provider, here is how you can handle it.
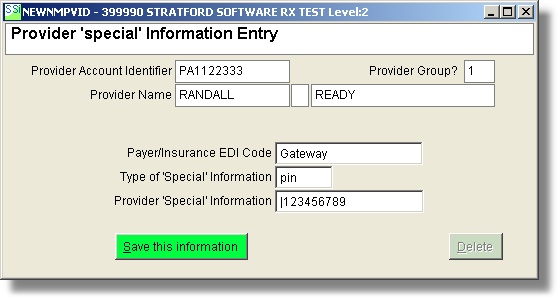
In this example, you are entering a special provider id for provider '01'. When a claim is sent to GatewayEDI, this provider special ID will be substituted for whatever you have in the provider screen.
Note: there may be a case where you do not want a provider ID to show in a specific box on the paper claim or in a specific segment in the EDI transmission file. In this case, you can leave the ID text box blank in the form above.
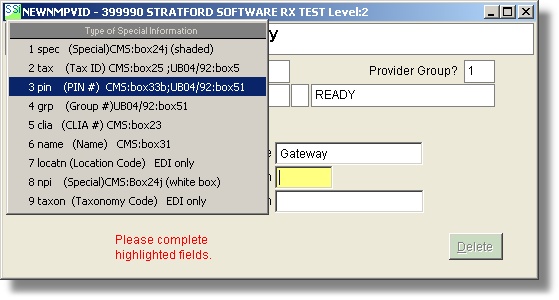
Select (PIN#) and it will put this special provider ID on the CMS 1500 form Box 33b
The setup below will print in box 33b a qualifier 'GG' and a special ID '123456789'
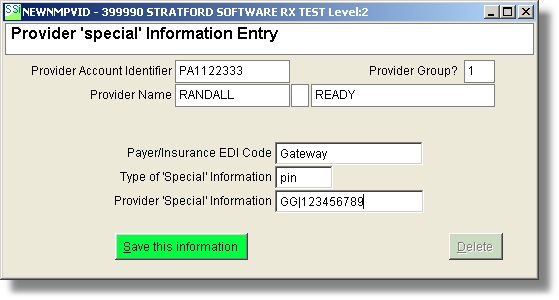
Note: if you have a case where the payer does not want a qualifier in front of the ID, you can simply delete that qualifier: (be sure to leave the separator bar '|' so the software will know that you are substituting a qualifier).