If you want to transmit a Claim status request to the payer/clearinghouse, you need to set up a 'form type' so you will have a selection on the insurance menu.
For the purpose of this topic, we will assume that you are using the form type 964 to transmit an ANSI 837 transaction set (claim) to your Medicare payer. To make things easier, we will use the same control files for the ANSI 276 transaction set (claim status request).
We understand that this topic is fairly 'technical' and not all of you will be able to follow it. If you call support they will help you. Also, you could send an email with your questions. We prefer the email because that would help us make this topic easier to follow.
Setting up a form type for the ANSI 276 Claim Status request/inquiry
From the main menu, select #8, then #5, then #8 "Form Type Setup"
From the "Form maintenance" menu select #4 EDI Program/Form Setup. See if you have the 964-S (the 'S' is for status) form type. If not, you need to set it up.
Press the Add New button. Set it up like this:
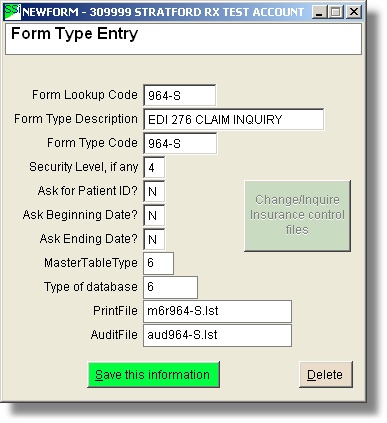
Note that you will not be able to enter the PrintFile or AuditFile name. Those will be created automatically when you save the information.
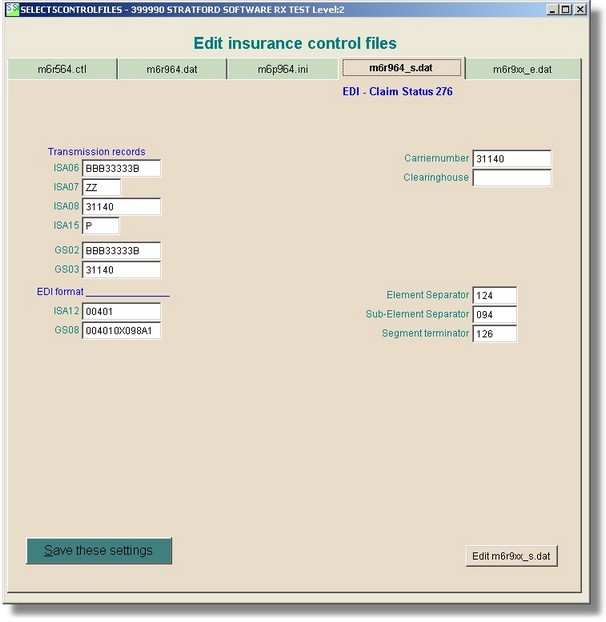
You may need to set up some special transmission information. To do that you will need to change the insurance control screen.